HLA Typing Test

What is the HLA Typing use for?
Laboratory testing for HLA is commonly used to determine transplant compatibility because different individuals may have very different HLA alleles, which may cause alloreactivity between recipients and donors.
HLA typing is a medical test to identify an individual's HLA (Human Leukocyte Antigen) antigens, which are proteins on the surface of cells that play a crucial role in the immune system. It is not a preventive maintenance test, but rather a test used for various medical purposes, most commonly in organ transplantation to ensure compatibility between donor and recipient.
Here's a more detailed explanation:
- HLA typing identifies the specific HLA antigens an individual possesses, which are unique markers for each person.
- Organ Transplantation: HLA matching is vital for successful organ transplantation, as it helps prevent the recipient's immune system from rejecting the transplanted organ.
- Bone Marrow Transplantation: HLA typing is also important for bone marrow transplantation, as it helps to ensure the compatibility between the donor and recipient.
- Other Medical Applications: HLA typing can also be used to diagnose certain autoimmune diseases and to assess the risk of developing certain diseases.
- Organ Transplantation: HLA matching is vital for successful organ transplantation, as it helps prevent the recipient's immune system from rejecting the transplanted organ.
- HLA typing is typically performed using a blood sample or a cheek swab.
- No, HLA typing is not a preventive maintenance test. It is a diagnostic test used to assess an individual's HLA antigens for medical purposes, such as organ transplantation or diagnosis of certain diseases.
HLA typing, also known as tissue typing, is a blood test that identifies antigens on the surface of cells and tissues, crucial for matching transplant recipients with compatible donors and assessing disease risks.
Here's a more detailed explanation:
- HLA typing is a genetic test that identifies specific proteins called human leukocyte antigens (HLA) found on the surface of cells, particularly white blood cells.
- Transplant Matching: HLA antigens are used by the immune system to distinguish between "self" and "non-self" cells. In transplantation, matching HLA types between a donor and recipient is crucial to prevent the recipient's immune system from attacking the transplanted tissue or organ.
- Disease Risk Assessment: Certain HLA types are associated with an increased risk of developing specific autoimmune diseases.
- Transfusion Support: HLA typing can help ensure that blood transfusions are compatible with the recipient's HLA type, reducing the risk of transfusion reactions.
- Transplant Matching: HLA antigens are used by the immune system to distinguish between "self" and "non-self" cells. In transplantation, matching HLA types between a donor and recipient is crucial to prevent the recipient's immune system from attacking the transplanted tissue or organ.
- Blood Sample: HLA typing typically involves taking a blood sample from the patient.
- Cheek Swab: Sometimes, a swab from the inside of the cheek (a buccal swab) can be used instead of a blood sample.
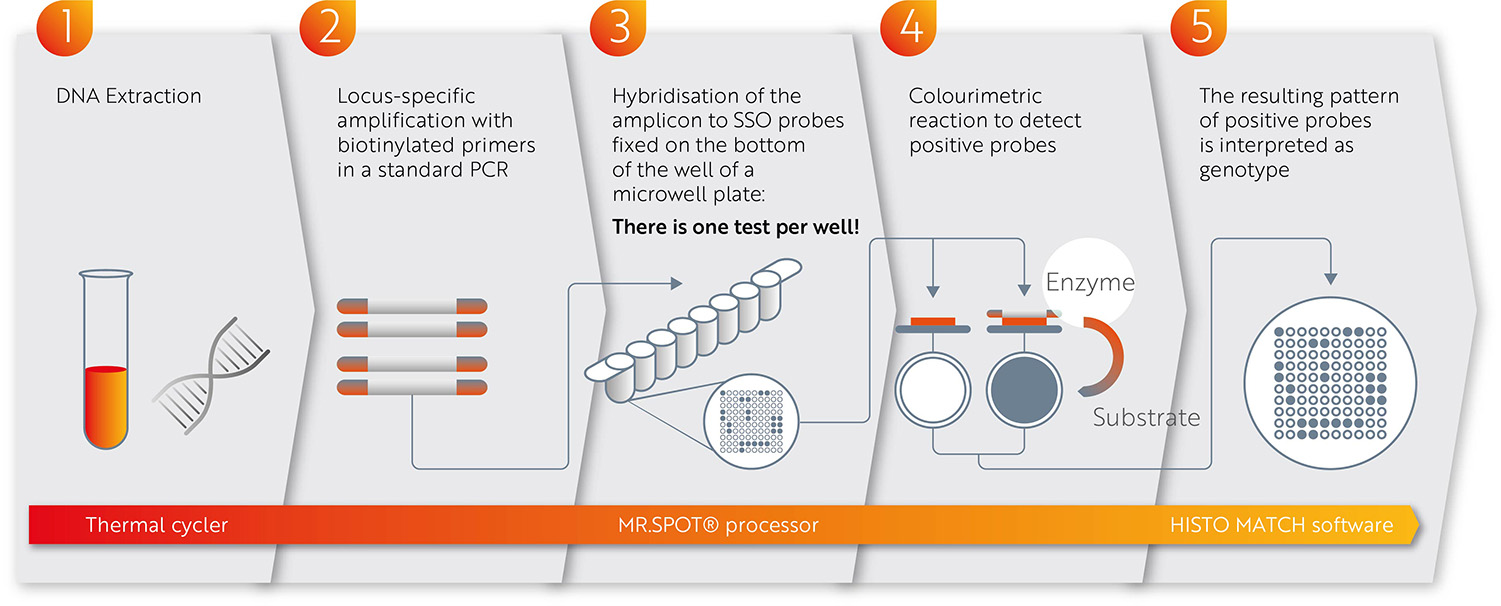
- Laboratory Analysis: The blood or swab sample is sent to a laboratory where it is analyzed to determine the patient's HLA type.
- Blood Sample: HLA typing typically involves taking a blood sample from the patient.
- Serological Typing: This method uses antibodies to identify HLA antigens.
- Molecular Typing: This method analyzes the DNA sequence of HLA genes.
- Serological Typing: This method uses antibodies to identify HLA antigens.
- Organ and Tissue Transplantation: HLA typing is essential for matching donors and recipients for organ and tissue transplants, such as kidney, liver, heart, and bone marrow transplants.
- Bone Marrow Transplantation: HLA typing is crucial for finding compatible bone marrow donors for patients with certain blood disorders or cancers.
- Disease Risk Assessment: HLA typing can help identify individuals at higher risk for certain autoimmune diseases, such as rheumatoid arthritis, ankylosing spondylitis, and type 1 diabetes.
- Forensic Identification: HLA typing can be used to help identify individuals in forensic cases.
- Parentage Testing: HLA typing was historically used for parentage testing, though more specific molecular tests are now available.
- Organ and Tissue Transplantation: HLA typing is essential for matching donors and recipients for organ and tissue transplants, such as kidney, liver, heart, and bone marrow transplants.
- Full Match: When a patient and donor share all the same HLA markers, it is considered a full match.
- Partial Match: When a patient and donor share some but not all of the same HLA markers, it is considered a partial match.
- Mismatched: When a patient and donor do not share any of the same HLA markers, it is considered a mismatched.
- Full Match: When a patient and donor share all the same HLA markers, it is considered a full match.